Written by Stephen J. Ritz, D.O., CCHP

The Institute of Medicine’s (IOM) 1999 report, “To Err is Human: Building a Safer Health System,” was a seminal moment that brought attention to the alarming prevalence of medical errors and their impact on patient safety in the United States. The statistics presented in the report underscored the need for a systematic, evidence-based approach to enhance patient safety across the health care system.
In the realm of corrections, where health care and criminal justice intersect, similar principles can be applied to address the specific challenges inherent in this unique environment. This article explores the elements of developing and implementing a patient safety program in correctional settings, drawing inspiration from the lessons learned in the general US health care sector.
Understanding the Scope of the Problem
The IOM report revealed that errors within the US health care system contribute to a significant number of deaths and injuries annually. This revelation serves as a poignant reminder that patient safety is not limited to traditional health care settings but extends to correctional facilities as well.
In fact, correctional settings share similarities with hospitals as complex systems with numerous interconnected components, where the potential for errors increases with the complexity of the environment. Accordingly, the potential for errors in correctional settings – akin to hospitals – necessitates a proactive and comprehensive approach to patient safety.
The Importance of Patient Safety in Corrections
The National Commission on Correctional Health Care (NCCHC) emphasizes that improving patient safety is not merely a regulatory requirement, but is foundational to the mission of correctional health care operations. Recognized as a philosophy, a way of thinking, and a blueprint for operations, patient safety becomes a guiding principle for ensuring the well-being of individuals in custody. Embracing patient safety as a core philosophy can serve to instill a culture that prioritizes the health and well-being of incarcerated individuals.
Implementing Evidence-Based Approaches
The IOM report called for evidence-based, comprehensive approaches to improving patient safety in health care settings. Similarly, correctional health care can benefit from adopting evidence-based practices tailored to the unique challenges of the correctional environment.
Development of a Comprehensive Patient Safety Program
The development of a comprehensive patient safety program integrates evidence-based practices into the daily operations of correctional health care. The program is broad in scope but will serve to address specific challenges, such as infectious disease, medication administration, specific disease outcomes, mental health issues, and substance use disorders, with targeted interventions based on the latest evidence-based best practices.
The following list of components of a patient safety program can provide the bridge from the philosophy of patient safety to reality. The overarching goal of such a process focuses on patient safety by detecting and proactively preventing errors, and optimizing outcomes. Such a program will focus on the core elements of planning, collaboration, and continuous quality improvement (CQI) and can incorporate the following elements.
Needs assessment: Conduct a thorough assessment of the existing patient safety practices, infrastructure, and resources in each facility’s medical unit, identifying potential vulnerabilities and areas for improvement.
Leadership and governance: Collaborate with the facility’s administrative leadership to form a dedicated patient safety team comprised of medical staff, corrections officers, administrators, and other stakeholders. This team oversees the program’s development, implementation, and ongoing evaluation.
Policy and procedure development: Create clear, comprehensive patient safety policies and procedures that address medical care, medication management, emergency response, communication, and health care incident reporting within the facility.
Education and training: Periodic and ongoing training sessions for medical staff, corrections officers, and other relevant personnel. These trainings cover topics such as patient safety principles, error recognition, incident reporting, communication strategies, and conflict resolution.
Incident reporting and analysis: Implement a confidential and non-punitive incident reporting system that encourages all staff to report errors and near-misses without fear of reprisal; This also would include mechanisms and processes which will analyze all reported incidents in order to identify trends, root causes, and recurring issues.
Risk assessment and mitigation: Perform regular, periodic risk assessments to identify potential hazards such as medication errors, improper medical procedures, or security-related challenges. For each identified risk, a mitigation strategy can be developed.
Medication safety: Establish protocols for medication administration, storage, and reconciliation, including leveraging technologies such as barcode scanning to ensure accurate medication administration and to prevent errors.
Communication and information sharing: Facilitate processes which outline clear and effective communication among medical staff, corrections officers, and other relevant personnel; this includes implementing structured handoff processes for shift changes and patient transfers.
Continuous quality improvement: A patient safety program can be an integral component of comprehensive CQI initiatives, to assess the effectiveness of the patient safety strategies. Data-driven insights from incident reports and performance metrics can be used to identify areas for improvement.
Patient engagement: Within the security restrictions present in a correctional environment, patients can be actively involved in their own safety by educating them about their rights, responsibilities, treatment plans, and how to advocate for their health care needs.
Audits and inspections: Conduct regular internal audits and external inspections to evaluate the program’s adherence to patient safety policies and procedures.
Crisis response plan: A patient safety team will be directly involved in the development of crisis response plans for issues such as medical emergencies, natural disasters, and pandemic disease outbreaks. Periodic and ongoing trainings and drills can help ensure that all staff members are well-versed in these protocols.
Data analytics and reporting: Data analytics can be utilized to track key patient safety metrics; to measure progress and make informed decisions; and to generate regular reports for facility leadership and the patient safety committee. One method to make such analytical data accessible and relevant is in the use of a clinical dashboard (see below).
Accountability: Maintaining transparency by regularly sharing the progress and outcomes of patient safety initiatives with internal and, when applicable, external stakeholders can enhance trust in the process and facilitate buy-in.
Sustainability and evolution: A robust patient safety process should have built-in components that serve to continuously assess the effectiveness of itself. Patient safety programming should allow adaptability based on the changing needs of facilities, emerging technologies, and evolving best practices in both the broader health care system, and corrections specifically.
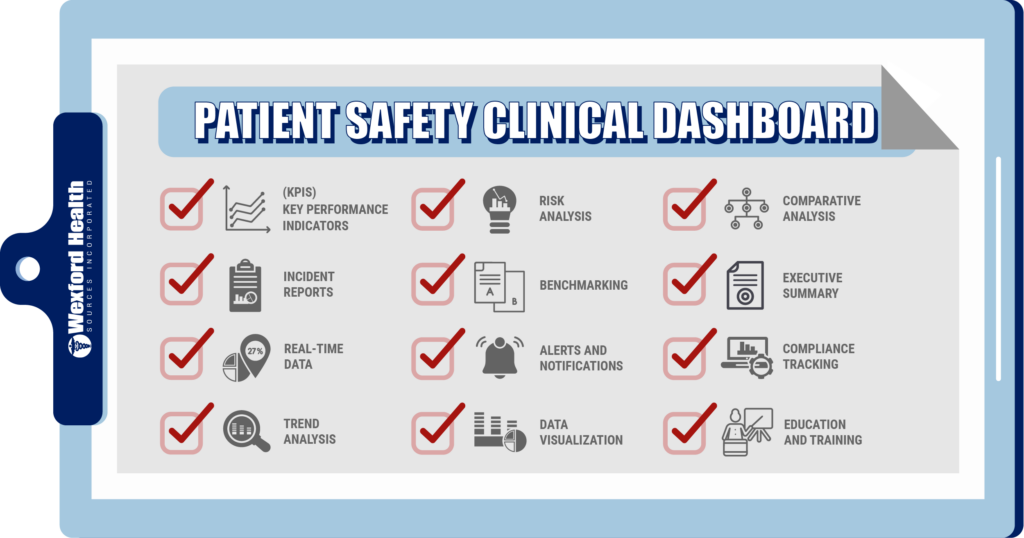
Patient Safety Clinical Dashboard
A patient safety clinical dashboard is a tool used in health care settings to monitor and manage patient safety initiatives and outcomes. It provides a visual representation of various patient safety metrics and indicators to help health care professionals and other stakeholders make informed decisions, and identify areas for improvement.
The components of a patient safety clinical dashboard can vary and will be tailored to the specific goals and needs of the facility, and the broader corrections system. Some common components include the following
- Key Performance Indicators (KPIs): These are the core metrics that reflect patient safety outcomes and initiatives. Examples include medication errors, facility-acquired infections, adverse events, near misses, and hospital/infirmary readmission rates.
- Incident Reports: Display data on incidents, errors, and adverse events that have been reported within the facility. This information helps identify patterns, root causes, and potential areas for improvement.
- Real-time Data: Display current patient safety information in real-time or close to real-time. This allows stakeholders to respond promptly to emerging issues.
- Trend Analysis: Display historical data and trends over time for various patient safety indicators. This helps identify trending in both improvements or worsening patient safety outcomes.
- Risk Assessment: Provide tools to assess and quantify the level of risk associated with different patient safety issues. This can aid in prioritizing interventions.
- Benchmarking: Compare the organization’s patient safety performance with national or industry standards such as those from NCCHC and ACA. This helps identify areas where the organization may be falling behind or excelling.
- Alerts and Notifications: Send automatic alerts and notifications when specific thresholds or criteria are met. This can help staff to respond quickly to critical situations or concerning trends.
- Data Visualization: Charts, graphs, heat maps, and other visualizations can be utilized to present data in an easily understandable format. This aids in identifying trends and patterns quickly.
- Comparative Analysis: Provide the ability to compare patient safety metrics across different departments, units, or facilities within the organization. This can highlight variations and areas for improvement.
- Executive Summary: A summary section that highlights the overall patient safety performance, recent improvements, ongoing challenges, and future goals.
- Compliance Tracking: Monitor compliance with patient safety protocols, guidelines, and best practices.
- Education and Training: Provide links to educational resources and training materials related to patient safety for continuous improvement.
The lessons learned from the IOM report in 1999 continue to resonate in various sectors, including corrections. Patient safety is not confined to traditional health care settings, and correctional facilities should recognize and address the unique issues they face.
The daunting challenges of patient safety can be approached in an organized and structured manner, building processes which consider several key elements, and made accessible to all stakeholders by use of a clinical dashboard.
By embracing patient safety as a core philosophy and implementing structured, organized, and evidence-based approaches, correctional systems and their individual facilities can build safer health care systems that align with the fundamental principles outlined by the IOM.
Written by Stephen J. Ritz, D.O., CCHP, Chief Medical Officer for Wexford Health Sources, Inc.
- Institute of Medicine (US) Committee on Quality of Health Care in America. To Err is Human: Building a Safer Health System. Kohn LT, Corrigan JM, Donaldson MS, editors. Washington (DC): National Academies Press (US); 2000. PMID: 25077248.
- Murphy DR, Savoy A, Satterly T, Sittig DF, Singh H. Dashboards for visual display of patient safety data: a systematic review. BMJ Health Care Inform. 2021 Oct;28(1): e100437. doi: 10.1136/bmjhci-2021-100437. PMID: 34615664; PMCID: PMC84963
- NCCHC Patient Safety White paper; Marc F. Stern, MD, MPH, FACP Revised February 8, 2023 -https://www.ncchc.org/wp-content/uploads/Patient-Safety-2016-Feb-2023.pdf

Recent Comments